When I work with couples who are recovering from sex and love addiction, one of the most common concerns is what to do when the betrayed partner gets triggered. This is especially relevant when the addict has achieved sobriety and is working their program, but the betrayed partner continues to experience triggers. A trigger is a reminder in the present of the addict’s hurtful and addictive behaviors in the past. Triggers can be accompanied by strong expressions of emotion that seem out of proportion to the present situation, flashbacks to the addict’s past behaviors, intense anxiety or fear, or a level of disgust toward the addict.
Triggers aren’t necessarily indicators that the addict has done anything wrong or broken their sobriety. In fact, triggers will come up no matter how long the addict has been sober. I often characterize triggers as having “one foot in the past and one foot in the present”. Though the addiction may not be happening currently, the feeling aroused by the trigger is the same as if it were happening in the present. They are a normal part of betrayal trauma recovery and broken trust that needs to be dealt with and healed in the relationship.
Types and Signs of Triggers
A trigger can be directly tied to the recovering addict’s behavior, but triggers can also be environmental. Triggers tied directly to the addict might be observing their interactions with the opposite sex, seeing your partner hide something on their phone or computer, or your spouse arriving home later than expected. An example of an environmental trigger might be a billboard for an adult bookstore, an explicit scene in a TV show or movie, or the mention of an affair in a book or magazine.
Sometimes these triggers lead to suspicion and distrust of the spouse, especially when patterns of behavior that were used to hide addiction are noted. For example, if the addict would often engage in sexual acting out behaviors while traveling for work, traveling will likely carry a trigger in the future. Or if the spouse used pornography late at night, staying up late alone may be another trigger.
Other times triggers are tied to relational dynamics that were present during the addiction. If defensiveness was used to hide addictive behavior or emotional disengagement occurred as a result of the addiction, these will likely stir up a trigger response. Emotional manipulation and gaslighting, withdrawing after an argument, and rage/intense anger are all types of relational dynamics that may have been used to hide or distract from the addictive behavior in the past. If they recur, they can remind the betrayed spouse of that experience and arouse suspicion.
As mentioned earlier, triggers often bring strong emotional reactions, to extremes of rage or the silent treatment. They can spiral the betrayed partner into destructive thought patterns and anxiety, which may lead to a return to safety-seeking behaviors. Examples of these include searching through emails or phones or numbing out with the betrayed partner’s own addiction to food, shopping, alcohol, or other compulsive or impulsive behaviors.
Some triggers are easier to prepare for, such as the travel trigger mentioned above. However, many times triggers come on unexpectedly. Having a plan in place for how you will respond to triggers as a couple can help you be prepared even for those that are unpredictable and arise without warning.
A Plan for the Addict
Slow down and breathe.
When your partner is triggered, often the impulse is to defend yourself against what can feel like an attack or accusation of wrongdoing. Unfortunately, this can intensify the triggering experience, adding even more distrust to the relationship as you repeat patterns of defensiveness or dismissal that were used to hide the addiction.
Instead, use the tool of your breath to slow yourself down before you jump on the defense. Take five to ten slow, deep abdominal breaths to help you stay present in your body and prepare to listen to their experience.
Remember what is happening.
Reframe these trigger moments as opportunities to grow in trust. Consider the concept that a trigger is about having one foot in the present and one foot in the past. Typically, the trigger is not about what is happening now and is more about what your actions were then. The trigger doesn’t necessarily carry an accusation with it, as much as it is a flashback to what happened in the past. If there is some truth to the accusation, it does need to be addressed, and we’ll explore that later.
Listen.
Turn your attention toward your spouse and actively hear what they are saying. It may help you to repeat their words back to them to ensure you understand, as well as clear up any misinterpretations or confusing communication. This also helps your partner feel heard and have the opportunity to clarify their perspective.
Contain the shame.
This is the most crucial component of this process for the addict. Triggers stir up shame because shame comes with facing the reality of the harm caused by your addictive behaviors. In fact, shame often contributed to addiction in the first place, as the addiction was a way to self-medicate against the pain of shame.
Addicts defend against shame in a multitude of ways. You might deny your addiction altogether, avoid reminders of the harm done by your addiction, focus more on the future than the past, or even repress or forget moments from the addiction. All of these options deny your personal responsibility, which can lead your betrayed partner to feel minimized.
In order to respond to your betrayed partner with empathy, you need to contain your experience of shame by separating your identity from what you have done. You need to remind yourself that you are not your addiction. This is work that can be done in therapy or with your sponsor in 12 Step. The ultimate goal is to take responsibility and remember that a trigger is not a threat to who you are.
Validate the pain of the past.
Connect with your spouse by acknowledging the reality of betrayal they faced at your hands and the hands of your addiction. Key phrases for this step include words like, “Of course you would feel that way” and, “It makes sense why you would feel _____ based on my past behaviors.”
Incorporate empathy here if you can. Words like, “That really stinks” or, “I’m so sorry you have to go through that, it sounds really hard” can be helpful here as well. A combination of validation and empathy will go far in defusing the tension of the trigger.
Examine your own behavior and apologize if needed.
Self-reflect to see if the trigger your betrayed partner is experiencing is based in anything for which you can take responsibility. A trigger like passing a billboard or going on work travel aren’t necessarily your responsibiilty, so this may be a situation to simply validate and share empathy.
On the other hand, triggers related to emotional manipulation in arguments, not following through on promised actions, or inappropriate behavior with a member of the opposite sex likely require an apology.
In a more subtle direction, it is important to apologize for safeguards that could have been in place to protect against this trigger. For example, perhaps the two of you agreed to make a plan before travel to connect during the trip and you failed to do so. Or you’ve committed to taking responsibility initiating date nights or weekly recovery check-ins, but you haven’t been consistent in following through on those commitments. Own your actions that set up an environment for a trigger.
Answer their questions.
See if your spouse has any follow-up questions to the trigger, particularly if it involved direct action or inaction on your part. Answer these questions as openly and honestly as you can. Remember that any deception here will come back to hurt you when the truth eventually gets revealed, as it inevitably will.
Rebuild trust in the moment.
Ask your partner if there is anything you can do to rebuild trust in the moment. Physical touch may be a good way to increase connection, if the partner desires it. They may also have a request for a date night or other shared activity as a way to connect emotionally and relationally. They may have a request to create a new agreement around the trigger for the future.
A Plan For the Partner
Breathe.
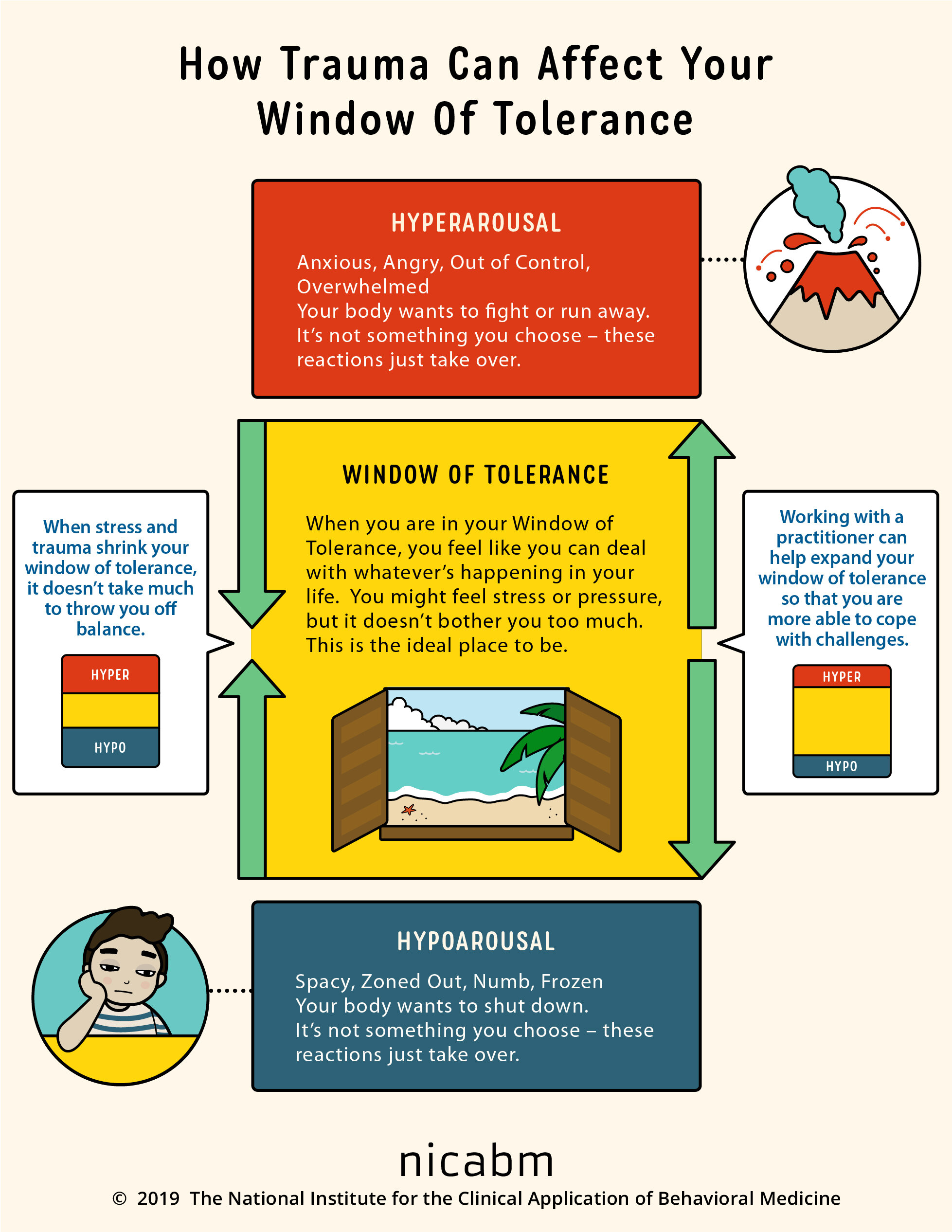
Just as the addict in this situation needs to slow down and connect to their body, the same is true for you. Intense emotions that accompany triggers can either take you completely out of your body or overwhelm your body with emotion. This is true for anyone facing trauma flashbacks. Practicing a centering or grounding breathing exercise can help you slow down enough to observe what is happening in your mind and body.
Reach out for support.
Get in contact with some of the support individuals in your life who know about your betrayal trauma recovery and ask for encouragement or a listening ear. A source for this support might come from a women’s support group, your therapist, or a close friend who is empathetic and supportive in your recovery. If you don’t have this support in place, now might be a good time to look for resources in your area or online that you can rely on the next time you face a trigger like this one.
Avoid the impulse to safety-seek.
Triggers that remind you of the addict’s past behaviors can throw you into repetition of the panic, fear, and hypervigilance of the early days after discovery. Safety-seeking behaviors include actions such as compulsively searching through your spouse’s internet search history, phone contacts, or emails. It could be manipulating your conversations with them to try to get them to slip up and say something incriminating.
Hallmarks of safety-seeking behaviors are that they are secretive, often carry shame with them, are attempts to feel like you have all the information and are in control, and usually make you feel worse instead of better. Instead of choosing these destructive patterns, lean into supportive self-care until you are able to have a conversation with a support person or with your spouse.
Approach your spouse with the talking formula.
When you feel affected by a trigger and it feels appropriate to do so, talk about it with the addict using this format: “When I heard/saw [the trigger], what went through my mind was [thoughts] and I felt [emotion word].”
Feel free to ask questions or confirmation about their behavior. For example, if it would help you to have more information, you might ask, “Would you be willing to share more about what was going on that day?” Or if you need reassurance of their recovery, you might say, “It would be helpful to be reminded of your recovery plan. Can we go through that together again?”
Make a request for a change in behavior, if needed.
Identify if you would like to approach future trigger moments differently as a result of what you learned from this one. Adapting your plan can involve both a joint discussion and an individual reflection. You might ask your partner, “Could we make a plan together for situations like this in the future?”
You can also identify relationship patterns that you’d like to change if they were involved in the trigger. For example, instead of emotional withdrawal and detachment, you could request that your partner remain present or plan a time to come back together to discuss an issue.
Practice self-care.
Riding on the roller-coaster of a trigger is not an easy process. It can be emotionally and physically exhausting to both experience a trigger and to process it in the aftermath. Practice activities that are self-soothing and bring a sense of peace and calm to your physical body. Utilize your resources of support to help you process through the conversation you had with your partner. Regardless of what happens in the conversation with your spouse, you can still care for and validate yourself.